This article is for any optometry student starting their clinical rotations. Trust me I’ve been there – palms sweaty, knees weak, arms heavy. As a newly minted graduate, I complied a guide on how to prepare for your externship as a student doctor.
Review these common conditions you will encounter in the clinic and make sure how to spot them. The next learning step is to think about treatment and management. Move on from “what is this?” to “what now?”
Most of the time, patients want to know how you’re going to treat their disease instead of the actual disease. You will be evolving as a student doctor because you won’t just be collecting information, you will be interpreting data and thinking about management.
5 Common Conditions to Understand Well in Clinic:
- Refractive Error & Troubleshooting

- Patients coming into the clinic may only want an updated prescription so learn how to refract well. But, we know an eye exam is much more than that. If they have an ocular disease, their refraction may be incorrect
- If there’s a large change in a patient’s refraction, quickly look through the slit lamp and find a cause, such as a myopic shift due to cataracts
- If a patient is diabetic, check if their sugars are well controlled before finalizing a prescription
- If they are young and there’s a large change, have a discussion with the parents about myopia control (Soft contact lenses, orthokeratology, atropine)
- Dry Eye Disease

- Dry Eye is often overlooked in eye exams. Be sure to look for signs of meibomian gland dysfunction, blepharitis and demodex in all patients. If the patient has signs, make sure to address them even if they are asymptomatic. Taking preventative measures are important to maintain the health of the ocular surface
- Examine the meibum by gently pressing against the lower eyelid and assess its quality and the level of inspissation
- Carefully assess and treat for dry eyes before referring for refractive or cataract surgery. If a patient is interested in refractive surgery, look for signs of dry eyes and make sure to have a conversation about the risk of neuropathic dry eyes
- If you are interested in learning more about dry eyes, I would highly recommend reading the TFOS DEWS II – Executive Summary Report
- Cataracts

- Understand the different types of cataracts and differentiate them with an optic section. With an optic section, you can distinguish each part of the lens (anterior, cortex, nucleus, posterior)
- Make sure to have an early discussion about surgery with the patient if they have indications for surgery complications (ex. Pseudoexfoliation)
- Glaucoma
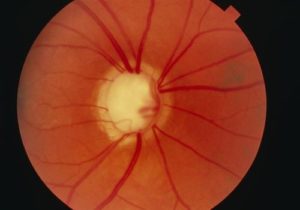
- Utilize your gonioscopy lens as much as possible. It’s especially important to assess for narrow angles to determine safe dilation and to differentiate between primary and secondary types of glaucoma
- Analyze visual fields and OCTs like a radiologist. Don’t assume red means glaucomatous or green means non-glaucomatous. Read Avoiding Clinical Misinterpretation and Artifacts of Optical Coherence Tomography Analysis to become an expert OCT interpreter. Reviewing these test properly is essential for diagnosing glaucoma and its management
- Diabetic Retinopathy

- Remember that diabetic retinopathy is divided into non-proliferative and proliferative. Non-proliferative diabetic retinopathy is classified as mild, moderate and severe. Review the management and follow up times for each grading
- Make sure to communicate any diabetic eye changes to your patient’s family physician or endocrinologist. A total team approach is needed through medications, proper diet and exercise to control diabetes
- If your patient has poor VA’s, make sure to rule out macular edema because it can present at any stage
- Check out this article on how to diagnose and manage diabetic retinopathy
Of course, this is a non-exhaustive list of common things seen in clinic so make sure to review other divisions of optometry such as speciality contact lenses and binocular vision.
Next Steps: Become comfortable with diagnostic imaging

Review the fundamentals of spotting abnormalities in fundus photography and OCT. Master these skills and quiz yourself with your friends.
PS. All of this content is free (the only word a student wants to hear).
- Fundus photography
- OCT
The journey to becoming a student doctor can feel daunting, but embrace the challenges you may face. Take the time to ask questions and investigate your patients cases. You’ll look back and be amazed at your ability to learn so much in a few months. Best of luck in clinic and feel free to reach out to me anytime.
Diana Nguyen, O.D.
Class of 2020